Coverage Selection
- Visit www.1enrollment.com/hpma to set up your account.
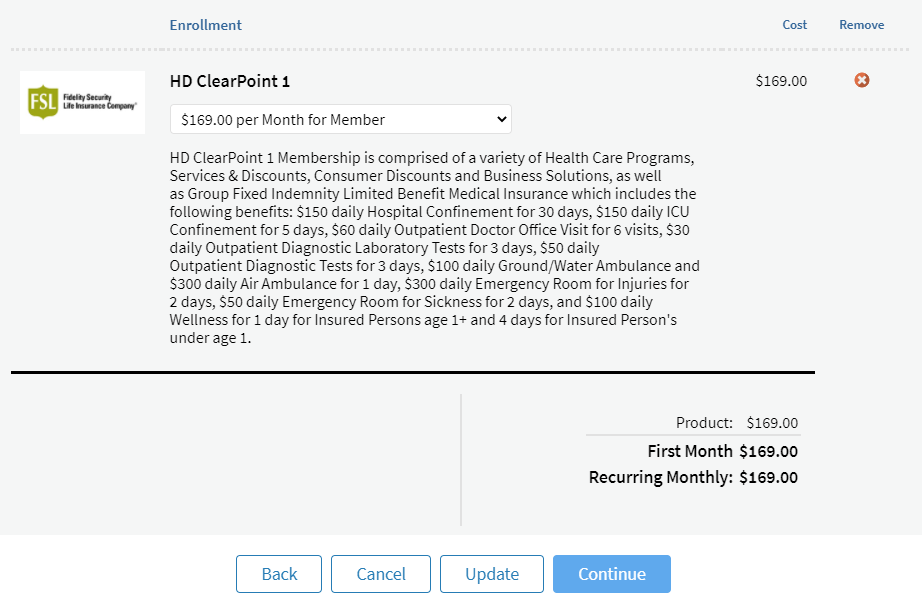
- Click Enroll on your first selection
- Select coverage level on dropdown
- Scroll down to bottom of page for additional selections
- Verify coverage level is correct for each product
- Click Continue
Check Out
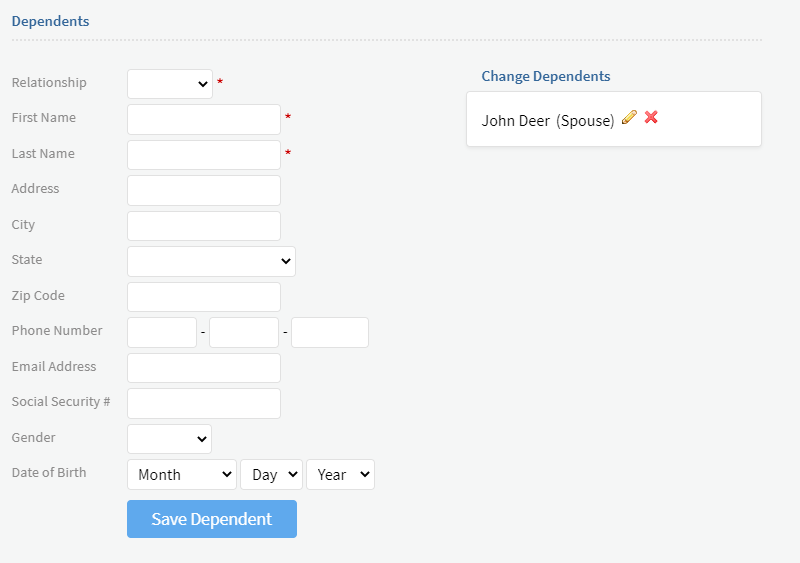
- Complete required information denoted by red asterisk
- Review effective date(s) for each product
- Fill out and click Save Dependent for each dependent
- Completed dependents will show up on the right side of the screen
- Review and Check the Authorization Section
Verification
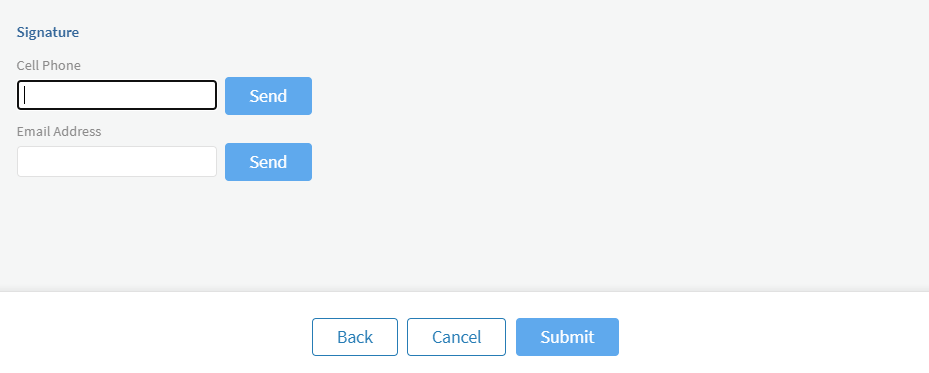
- Click Send Link under Signature and fill in Cell Phone or Email
- Review, Approve and Sign Your Document message will be sent to Cell Phone or Email
- Review your enrollment information, check any applicable boxes, sign, type your name and click Accept
- Go back to enrollment site and wait until you see Signature Document Received in a green box
- Click Submit and you will see a Confirmation screen
Immediately upon enrollment, you will receive a Welcome Email for each product you selected with details on your membership.
For any questions during the Enrollment process, please contact Member Services at (214) 436-8869.
Around the clock, lifesaving air medical transport is there for you
What if a medical emergency occurred while you were hours from home – or halfway around the globe? It’s a frightening situation that happens all too often. Fortunately, select Health Depot memberships include air medical transportation coverage from AirMed. Wherever you are and whatever the medical need, you have seamless access to the highest level of acute care provided by the leading air medical company in North America.
Around the clock and around the globe, AirMed transports you or your covered dependents to the hospital of your choice as quickly as possible. AirMed maintains a fleet of dedicated medical aircraft -- ICU-equipped jets, all staffed with highly trained doctors, nurses and respiratory therapists. It offers the most experience in the industry, having completed 20,000- plus missions spanning 150 countries. And, it is the only provider with every major worldwide certification, including U.S. Department of Defense air carrier status.
Critical Advantages
- The fastest and safest transport – Founded on top-notch medical logistics across the globe
- Worldwide medical evacuation – Transport back to the patient’s hospital of choice whether abroad or as close as 150 miles from home
- Commercial medical assistance – For situations when a patient has the ability to travel commercially but requires medical assistance
- 24/7 medical services hotline – On-call nursing staff answer medical-related questions day and night
- Transportation of mortal remains – Even in the worst circumstances, count on AirMed for expert, compassionate logistics and care
Coordinated Response
From the second you contact AirMed, a team of seasoned experts springs into motion. It immediately begins all necessary coordination of your medical, security or transport needs. You or your dependents are covered with these services 24/7/365:
- Access to a medical consultant
- Pre-trip planning assistance
- Your choice of hospital
- Dedicated patient advocacy
- Arranged medical transport
- Advice on security risks
At home or abroad, the entire suite of AirMed medical transport benefits is available to Health Depot members on select membership levels without deductibles, claim forms or out-of-pocket expenses.

How Does the PPO Network Work?
This plan allows members to select any dentist of their choice. When services are provided by an in-network provider, out-of-pocket costs will generally be less than if performed by an out-of-network provider. Services performed out-of-network will be paid based on fee schedule given for each procedure.
In-network benefits are administered by providers who participate in our nationwide argusChoice PPO network. This network encompasses dentists in any of the following networks: DenteMax, Maverest, Connection Dental, Premier, TDA and Healthmart. The argusChoice PPO network has more than 275,000 access points across the United States. When verifying coverages and networks with providers, members need to refer to all the networks listed above.
Out-of-network benefits may also receive applicable network discounts from providers in networks under an agreement with NovaNet, a national network program.
What is a Network Dentist?
Network dentists agree to accept argusChoice PPO’s discounted fees as payment in full for covered services. Non-network dentists can charge you more. This means you will lower your out-of-pocket expense using a network dentist.
You can receive care from any licensed dentist. But your benefits may differ and your out-of-pocket costs could be higher with a non-network dentist.
Locate Participating Providers
Visit https://argusdental.com/find-a-provider and select argusChoice PPO network to locate participating providers.
Health Care Discounts Disclosure
Not available in AK, OK, UT, VT, WA. If you move to one of those states, your discount medical benefits will terminate.
The discount medical, health, and drug benefits of this Plan (The Plan) are NOT insurance, a health insurance policy, a Medicare Prescription Drug Plan or a qualified health plan under the Affordable Care Act. The Plan provides discounts for certain medical services, pharmaceutical supplies, prescription drugs or medical equipment and supplies offered by providers who have agreed to participate in The Plan. The range of discounts for medical, pharmacy or ancillary services offered under The Plan will vary depending on the type of provider and products or services received. The Plan does not make and is prohibited from making members' payments to providers for products or services received under The Plan. The Plan member is required and obligated to pay for all discounted prescription drugs, medical and pharmaceutical supplies, services and equipment received under The Plan, but will receive a discount on certain identified medical, pharmaceutical supplies, prescription drugs, medical equipment and supplies from providers in The Plan. You may call (214) 436-8882 or email customerservice@premierhsllc.com for more information or visit myhealthaccountmanager.com for a list of providers. The Plan will make available before purchase and upon request, a list of program providers and the providers’ city, state and specialty, located in the member’s service area. The fees for The Plan are specified in the membership agreement.
Note to MA consumers: The discount plan is not insurance coverage and does not meet the minimum creditable coverage requirements under M.G.L. c. 111M and 956 CMR 5.00.
HDCP1018-7
Health Care Discounts Disclosure
Not available in AK, IL, OK, UT, VT, WA. If you move to one of those states, your discount medical benefits will terminate.
The discount medical, health, and drug benefits of this Plan (The Plan) are NOT insurance, a health insurance policy, a Medicare Prescription Drug Plan or a qualified health plan under the Affordable Care Act. The Plan provides discounts for certain medical services, pharmaceutical supplies, prescription drugs or medical equipment and supplies offered by providers who have agreed to participate in The Plan. The range of discounts for medical, pharmacy or ancillary services offered under The Plan will vary depending on the type of provider and products or services received. The Plan does not make and is prohibited from making members' payments to providers for products or services received under The Plan. The Plan member is required and obligated to pay for all discounted prescription drugs, medical and pharmaceutical supplies, services and equipment received under The Plan, but will receive a discount on certain identified medical, pharmaceutical supplies, prescription drugs, medical equipment and supplies from providers in The Plan. You may call (214) 436-8882 or email customerservice@premierhsllc.com for more information or visit myhealthaccountmanager.com for a list of providers. The Plan will make available before purchase and upon request, a list of program providers and the providers’ city, state and specialty, located in the member’s service area. The fees for The Plan are specified in the membership agreement.
Note to MA consumers: The discount plan is not insurance coverage and does not meet the minimum creditable coverage requirements under M.G.L. c. 111M and 956 CMR 5.00.

